TELL ME ABOUT CANCER
MEN AND CANCER
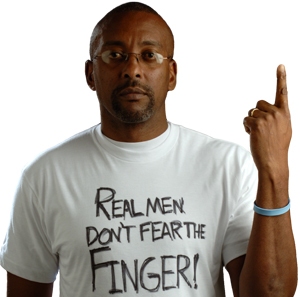
Testicular cancer
Sat, 13th August, 2011
is a type of cancer that develops in the testicle(s) of men. It is considered to be uncommon, with about 8,000 men diagnosed each year. The good news is that this type of cancer is highly treatable and curable.
Causes and Risk Factors of Testicular Cancer
Although researchers cannot pinpoint exactly what causes testicular cancer, they have identified several known risk factors for the disease. A risk factor is something that increases the likelihood that you may develop a disease, but is not a guarantee you will get it. Risk factors include:
•having had an undescended testicle, although if this is corrected early in life, the risk is reduced
•having had abnormal development of the testicles
•having a personal or family history of testicular cancer
•being diagnosed with Klinefelter's syndrome
•being infected with HIV
•being Caucasian
Testicular Cancer Symptoms
Common symptoms of testicular cancer include:
•painless lump in the testicle or both testicles; less commonly, the lump will cause pain
•heaviness, or feeling of swelling in the scrotum
•discomfort or pain in the scrotum
•ache in lower back, pelvis or groin area
•collection of fluid in the scrotum
Causes and Risk Factors of Testicular Cancer
Although researchers cannot pinpoint exactly what causes testicular cancer, they have identified several known risk factors for the disease. A risk factor is something that increases the likelihood that you may develop a disease, but is not a guarantee you will get it. Risk factors include:
•having had an undescended testicle, although if this is corrected early in life, the risk is reduced
•having had abnormal development of the testicles
•having a personal or family history of testicular cancer
•being diagnosed with Klinefelter's syndrome
•being infected with HIV
•being Caucasian
Testicular Cancer Symptoms
Common symptoms of testicular cancer include:
•painless lump in the testicle or both testicles; less commonly, the lump will cause pain
•heaviness, or feeling of swelling in the scrotum
•discomfort or pain in the scrotum
•ache in lower back, pelvis or groin area
•collection of fluid in the scrotum
Colon Cancer Treatment
Sat, 13th August, 2011
Treatment depends partly on the stage of the cancer. In general, treatments may include:
•Surgery (most often a colectomy) to remove cancer cells
•Chemotherapy to kill cancer cells
•Radiation therapy to destroy cancerous tissue
SURGERY
Stage 0 colon cancer may be treated by removing the cancer cells, often during a colonoscopy. For stages I, II, and III cancer, more extensive surgery is needed to remove the part of the colon that is cancerous. (See: Colon resection)
There is some debate as to whether patients with stage II colon cancer should receive chemotherapy after surgery. You should discuss this with your oncologist.
CHEMOTHERAPY
Almost all patients with stage III colon cancer should receive chemotherapy after surgery for approximately 6 - 8 months. The chemotherapy drug 5-fluorouracil has been shown to increase the chance of a cure in certain patients.
Chemotherapy is also used to improve symptoms and prolong survival in patients with stage IV colon cancer.
•Irinotecan, oxaliplatin, capecitabine, and 5-fluorouracil are the three most commonly used drugs.
•Monoclonal antibodies, including cetuximab (Erbitux), panitumumab (Vectibix), bevacizumab (Avastin), and other drugs have been used alone or in combination with chemotherapy.
You may receive just one type, or a combination of these drugs.
RADIATION
Although radiation therapy is occasionally used in patients with colon cancer, it is usually used in combination with chemotherapy for patients with stage III rectal cancer.
For patients with stage IV disease that has spread to the liver, various treatments directed specifically at the liver can be used. This may include:
•Burning the cancer (ablation)
•Delivering chemotherapy or radiation directly into the liver
•Freezing the cancer (cryotherapy)
•Surgery
•Surgery (most often a colectomy) to remove cancer cells
•Chemotherapy to kill cancer cells
•Radiation therapy to destroy cancerous tissue
SURGERY
Stage 0 colon cancer may be treated by removing the cancer cells, often during a colonoscopy. For stages I, II, and III cancer, more extensive surgery is needed to remove the part of the colon that is cancerous. (See: Colon resection)
There is some debate as to whether patients with stage II colon cancer should receive chemotherapy after surgery. You should discuss this with your oncologist.
CHEMOTHERAPY
Almost all patients with stage III colon cancer should receive chemotherapy after surgery for approximately 6 - 8 months. The chemotherapy drug 5-fluorouracil has been shown to increase the chance of a cure in certain patients.
Chemotherapy is also used to improve symptoms and prolong survival in patients with stage IV colon cancer.
•Irinotecan, oxaliplatin, capecitabine, and 5-fluorouracil are the three most commonly used drugs.
•Monoclonal antibodies, including cetuximab (Erbitux), panitumumab (Vectibix), bevacizumab (Avastin), and other drugs have been used alone or in combination with chemotherapy.
You may receive just one type, or a combination of these drugs.
RADIATION
Although radiation therapy is occasionally used in patients with colon cancer, it is usually used in combination with chemotherapy for patients with stage III rectal cancer.
For patients with stage IV disease that has spread to the liver, various treatments directed specifically at the liver can be used. This may include:
•Burning the cancer (ablation)
•Delivering chemotherapy or radiation directly into the liver
•Freezing the cancer (cryotherapy)
•Surgery
Colon Cancer Symptoms
Sat, 13th August, 2011
Many cases of colon cancer have no symptoms. The following symptoms, however, may indicate colon cancer:
•Abdominal pain and tenderness in the lower abdomen
•Blood in the stool
•Diarrhea, constipation, or other change in bowel habits
•Narrow stools
•Weight loss with no known reason
Signs and tests
With proper screening, colon cancer can be detected before symptoms develop, when it is most curable.
Your doctor will perform a physical exam and press on your belly area. The physical exam rarely shows any problems, although the doctor may feel a lump (mass) in the abdomen. A rectal exam may reveal a mass in patients with rectal cancer, but not colon cancer.
A fecal occult blood test (FOBT) may detect small amounts of blood in the stool, which could suggest colon cancer. However, this test is often negative in patients with colon cancer. For this reason, a FOBT must be done along with colonoscopy or sigmoidoscopy. It is also important to note that a positive FOBT doesn't necessarily mean you have cancer.
Imaging tests to screen for and potentially diagnose colorectal cancer include:
•Colonoscopy
•Sigmoidoscopy
Note: Only colonoscopy can see the entire colon, and this is the best screening test for colon cancer.
Blood tests that may be done include:
•Complete blood count (CBC) to check for anemia
•Liver function tests
If your doctor learns that you do have colorectal cancer, more tests will be done to see if the cancer has spread. This is called staging. CT or MRI scans of the abdomen, pelvic area, chest, or brain may be used to stage the cancer. Sometimes, PET scans are also used.
Stages of colon cancer are:
•Stage 0: Very early cancer on the innermost layer of the intestine
•Stage I: Cancer is in the inner layers of the colon
•Stage II: Cancer has spread through the muscle wall of the colon
•Stage III: Cancer has spread to the lymph nodes
•Stage IV: Cancer has spread to other organs
Blood tests to detect tumor markers, including carcinoembryonic antigen (CEA) and CA 19-9, may help your physician follow you during and after treatment.
•Abdominal pain and tenderness in the lower abdomen
•Blood in the stool
•Diarrhea, constipation, or other change in bowel habits
•Narrow stools
•Weight loss with no known reason
Signs and tests
With proper screening, colon cancer can be detected before symptoms develop, when it is most curable.
Your doctor will perform a physical exam and press on your belly area. The physical exam rarely shows any problems, although the doctor may feel a lump (mass) in the abdomen. A rectal exam may reveal a mass in patients with rectal cancer, but not colon cancer.
A fecal occult blood test (FOBT) may detect small amounts of blood in the stool, which could suggest colon cancer. However, this test is often negative in patients with colon cancer. For this reason, a FOBT must be done along with colonoscopy or sigmoidoscopy. It is also important to note that a positive FOBT doesn't necessarily mean you have cancer.
Imaging tests to screen for and potentially diagnose colorectal cancer include:
•Colonoscopy
•Sigmoidoscopy
Note: Only colonoscopy can see the entire colon, and this is the best screening test for colon cancer.
Blood tests that may be done include:
•Complete blood count (CBC) to check for anemia
•Liver function tests
If your doctor learns that you do have colorectal cancer, more tests will be done to see if the cancer has spread. This is called staging. CT or MRI scans of the abdomen, pelvic area, chest, or brain may be used to stage the cancer. Sometimes, PET scans are also used.
Stages of colon cancer are:
•Stage 0: Very early cancer on the innermost layer of the intestine
•Stage I: Cancer is in the inner layers of the colon
•Stage II: Cancer has spread through the muscle wall of the colon
•Stage III: Cancer has spread to the lymph nodes
•Stage IV: Cancer has spread to other organs
Blood tests to detect tumor markers, including carcinoembryonic antigen (CEA) and CA 19-9, may help your physician follow you during and after treatment.
Colon cancer
Sat, 13th August, 2011
Colorectal cancer; Cancer - colon; Rectal cancer; Cancer - rectum; Adenocarcinoma - colon; Colon - adenocarcinoma
Last reviewed: December 28, 2010.
Colon, or colorectal, cancer is cancer that starts in the large intestine (colon) or the rectum (end of the colon).
Other types of cancer can affect the colon, such as lymphoma, carcinoid tumors, melanoma, and sarcomas. These are rare. In this article, use of the term "colon cancer" refers to colon carcinoma only.
Causes, incidence, and risk factors
According to the American Cancer Society, colorectal cancer is one of the leading causes of cancer-related deaths in the United States. However, early diagnosis often leads to a complete cure.
Almost all colon cancer starts in glands in the lining of the colon and rectum. When doctors talk about colorectal cancer, this is usually what they are talking about.
There is no single cause of colon cancer. Nearly all colon cancers begin as noncancerous (benign) polyps, which slowly develop into cancer.
You have a higher risk for colon cancer if you:
•Are older than 60
•Are African American of eastern European descent
•Eat a diet high in red or processed meats
•Have cancer elsewhere in the body
•Have colorectal polyps
•Have inflammatory bowel disease (Crohn's disease or ulcerative colitis)
•Have a family history of colon cancer
•Have a personal history of breast cancer
Certain genetic syndromes also increase the risk of developing colon cancer. Two of the most common are:
•Familial adenomatous polyposis (FAP)
•Hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome
What you eat may play a role in your risk of colon cancer. Colon cancer may be associated with a high-fat, low-fiber diet and red meat. However, some studies have found that the risk does not drop if you switch to a high-fiber diet, so this link is not yet clear.
Smoking cigarettes and drinking alcohol are other risk factors for colorectal cancer.
Last reviewed: December 28, 2010.
Colon, or colorectal, cancer is cancer that starts in the large intestine (colon) or the rectum (end of the colon).
Other types of cancer can affect the colon, such as lymphoma, carcinoid tumors, melanoma, and sarcomas. These are rare. In this article, use of the term "colon cancer" refers to colon carcinoma only.
Causes, incidence, and risk factors
According to the American Cancer Society, colorectal cancer is one of the leading causes of cancer-related deaths in the United States. However, early diagnosis often leads to a complete cure.
Almost all colon cancer starts in glands in the lining of the colon and rectum. When doctors talk about colorectal cancer, this is usually what they are talking about.
There is no single cause of colon cancer. Nearly all colon cancers begin as noncancerous (benign) polyps, which slowly develop into cancer.
You have a higher risk for colon cancer if you:
•Are older than 60
•Are African American of eastern European descent
•Eat a diet high in red or processed meats
•Have cancer elsewhere in the body
•Have colorectal polyps
•Have inflammatory bowel disease (Crohn's disease or ulcerative colitis)
•Have a family history of colon cancer
•Have a personal history of breast cancer
Certain genetic syndromes also increase the risk of developing colon cancer. Two of the most common are:
•Familial adenomatous polyposis (FAP)
•Hereditary nonpolyposis colorectal cancer (HNPCC), also known as Lynch syndrome
What you eat may play a role in your risk of colon cancer. Colon cancer may be associated with a high-fat, low-fiber diet and red meat. However, some studies have found that the risk does not drop if you switch to a high-fiber diet, so this link is not yet clear.
Smoking cigarettes and drinking alcohol are other risk factors for colorectal cancer.
Prostate Cancer Treatment
Sat, 13th August, 2011
The best treatment for your prostate cancer may not always be clear. Sometimes, your doctor may recommend one treatment because of what is known about your type of cancer and your risk factors. Other times, your doctor will talk with you about two or more treatments that could be good for your cancer.
In the early stages, talk to your doctor about several options, including surgery and radiation therapy. In older patients, simply monitoring the cancer with PSA tests and biopsies may be an option.
Prostate cancer that has spread may be treated with drugs to reduce testosterone levels, surgery to remove the testes, or chemotherapy.
Surgery, radiation therapy, and hormonal therapy can interfere with sexual desire or performance. Problems with urine control are common after surgery and radiation therapy. These problems may either improve over time or get worse, depending on the treatment. Discuss your concerns with your health care provider.
SURGERY
Surgery is usually only recommended after a thorough evaluation and discussion of the benefits and risks of the procedure.
•Surgery to remove the prostate and some of the tissue around it is an option when the cancer has not spread beyond the prostate gland. This surgery is called radical prostatectomy. It can also be done with robotic surgery.
•Possible problems after the surgeries include difficulty controlling urine or bowel movements and erection problems.
RADIATION THERAPY
Radiation therapy uses high-powered x-rays or radioactive seeds to kill cancer cells.
Radiation therapy works best to treat prostate cancer that has not spread outside of the prostate. It may also be used after surgery, if there is a risk that prostate cancer cells may still be present. Radiation is sometimes used for pain relief when cancer has spread to the bone.
External beam radiation therapy uses high-powered x-rays pointed at the prostate gland.
•It is done in a radiation oncology center usually connected to a hospital. You will come to the center from home 5 days a week for the treatments. The therapy lasts for 6 -8 weeks.
•Before treatment, a therapist will mark the part of the body that is to be treated with a special pen.
•The radiation is delivered to the prostate gland using a device that looks like a normal x-ray machine. The treatment itself is generally painless.
•Side effects may include impotence, incontinence, appetite loss, fatigue, skin reactions, rectal burning or injury, diarrhea, bladder urgency, and blood in urine.
Prostate brachytherapy involves placing radioactive seeds inside the prostate gland.
•A surgeon inserts small needles through the skin behind your scrotum to inject the seeds. The seeds are so small that you don't feel them. They can be temporary or permanent.
•Brachytherapy is often used for men with smaller prostate cancer that is found early and is slow-growing.
•It also may be given with external beam radiation therapy for some patients with more advanced cancer.
•Side effects may include pain, swelling or bruising in your penis or scrotum, red-brown urine or semen, impotence, incontinence, and diarrhea.
Proton therapy is another kind of radiation used to treat prostate cancer. Doctors aim proton beams onto a tumor, so there is less damage to the surrounding tissue.
HORMONE THERAPY
Testosterone is the body's main male hormone. Prostate tumors need testosterone to grow. Hormonal therapy is any treatment that decreases the effect of testosterone on prostate cancer. These treatments can prevent further growth and spread of cancer.
Hormone therapy is mainly used in men whose cancer has spread to help relieve symptoms. There are two types of drugs used for hormone therapy.
The primary type is called a luteinizing hormone-releasing hormones (LH-RH) agonist:
•These medicines block the body from making testosterone. The drugs must be given by injection, usually every 3 - 6 months.
•They include leuprolide, goserelin, nafarelin, triptorelin, histrelin, buserelin, and degarelix.
•Possible side effects include nausea and vomiting, hot flashes, anemia, lethargy, osteoporosis, reduced sexual desire, decreased muscle mass, weight gain, and impotence.
The other medications used are called androgen-blocking drugs.
•They are often given along with the above drugs.
•They include flutamide, bicalutamide, and nilutamide.
•Possible side effects include erectile dysfunction, loss of sexual desire, liver problems, diarrhea, and enlarged breasts.
Much of the body's testosterone is made by the testes. As a result, removal of the testes (called orchiectomy) can also be used as a hormonal treatment. This surgery is not done very often.
Chemotherapy and immunotherapy are used to treat prostate cancers that no longer respond to hormone treatment. An oncology specialist will usually recommend a single drug or a combination of drugs.
MONITORING
After treatment for prostate cancer, you will be closely watched to make sure the cancer does not spread. This involves routine doctor check-ups, including serial PSA blood tests (usually every 3 months to 1 year).
In the early stages, talk to your doctor about several options, including surgery and radiation therapy. In older patients, simply monitoring the cancer with PSA tests and biopsies may be an option.
Prostate cancer that has spread may be treated with drugs to reduce testosterone levels, surgery to remove the testes, or chemotherapy.
Surgery, radiation therapy, and hormonal therapy can interfere with sexual desire or performance. Problems with urine control are common after surgery and radiation therapy. These problems may either improve over time or get worse, depending on the treatment. Discuss your concerns with your health care provider.
SURGERY
Surgery is usually only recommended after a thorough evaluation and discussion of the benefits and risks of the procedure.
•Surgery to remove the prostate and some of the tissue around it is an option when the cancer has not spread beyond the prostate gland. This surgery is called radical prostatectomy. It can also be done with robotic surgery.
•Possible problems after the surgeries include difficulty controlling urine or bowel movements and erection problems.
RADIATION THERAPY
Radiation therapy uses high-powered x-rays or radioactive seeds to kill cancer cells.
Radiation therapy works best to treat prostate cancer that has not spread outside of the prostate. It may also be used after surgery, if there is a risk that prostate cancer cells may still be present. Radiation is sometimes used for pain relief when cancer has spread to the bone.
External beam radiation therapy uses high-powered x-rays pointed at the prostate gland.
•It is done in a radiation oncology center usually connected to a hospital. You will come to the center from home 5 days a week for the treatments. The therapy lasts for 6 -8 weeks.
•Before treatment, a therapist will mark the part of the body that is to be treated with a special pen.
•The radiation is delivered to the prostate gland using a device that looks like a normal x-ray machine. The treatment itself is generally painless.
•Side effects may include impotence, incontinence, appetite loss, fatigue, skin reactions, rectal burning or injury, diarrhea, bladder urgency, and blood in urine.
Prostate brachytherapy involves placing radioactive seeds inside the prostate gland.
•A surgeon inserts small needles through the skin behind your scrotum to inject the seeds. The seeds are so small that you don't feel them. They can be temporary or permanent.
•Brachytherapy is often used for men with smaller prostate cancer that is found early and is slow-growing.
•It also may be given with external beam radiation therapy for some patients with more advanced cancer.
•Side effects may include pain, swelling or bruising in your penis or scrotum, red-brown urine or semen, impotence, incontinence, and diarrhea.
Proton therapy is another kind of radiation used to treat prostate cancer. Doctors aim proton beams onto a tumor, so there is less damage to the surrounding tissue.
HORMONE THERAPY
Testosterone is the body's main male hormone. Prostate tumors need testosterone to grow. Hormonal therapy is any treatment that decreases the effect of testosterone on prostate cancer. These treatments can prevent further growth and spread of cancer.
Hormone therapy is mainly used in men whose cancer has spread to help relieve symptoms. There are two types of drugs used for hormone therapy.
The primary type is called a luteinizing hormone-releasing hormones (LH-RH) agonist:
•These medicines block the body from making testosterone. The drugs must be given by injection, usually every 3 - 6 months.
•They include leuprolide, goserelin, nafarelin, triptorelin, histrelin, buserelin, and degarelix.
•Possible side effects include nausea and vomiting, hot flashes, anemia, lethargy, osteoporosis, reduced sexual desire, decreased muscle mass, weight gain, and impotence.
The other medications used are called androgen-blocking drugs.
•They are often given along with the above drugs.
•They include flutamide, bicalutamide, and nilutamide.
•Possible side effects include erectile dysfunction, loss of sexual desire, liver problems, diarrhea, and enlarged breasts.
Much of the body's testosterone is made by the testes. As a result, removal of the testes (called orchiectomy) can also be used as a hormonal treatment. This surgery is not done very often.
Chemotherapy and immunotherapy are used to treat prostate cancers that no longer respond to hormone treatment. An oncology specialist will usually recommend a single drug or a combination of drugs.
MONITORING
After treatment for prostate cancer, you will be closely watched to make sure the cancer does not spread. This involves routine doctor check-ups, including serial PSA blood tests (usually every 3 months to 1 year).
Prostate Cancer Signs and tests
Sat, 13th August, 2011
Prostate biopsy is the only test that can confirm the diagnosis. Tissue from the prostate is viewed underneath a microscope. Biopsy results are reported using something called a Gleason grade and a Gleason score.
The Gleason grade is how aggressive the prostate cancer might be. It grades tumors on a scale of 1 - 5, based on how different from normal tissue the cells are.
Often, more than one Gleason grade is present within the same tissue sample. The Gleason grade is therefore used to create a Gleason score by adding the two most predominant grades together (a scale of 2 - 10). The higher the Gleason score, the more likely the cancer is to have spread beyond the prostate gland:
•Scores 2 - 4: Low-grade cancer
•Scores 5 - 7: Intermediate- (or in the middle-) grade cancer. Most prostate cancers fall into this category.
•Scores 8 - 10: High-grade cancer (poorly-differentiated cells)
There are two reasons your doctor may perform a prostate biopsy:
•Your PSA blood test is high. See also: PSA
•A rectal exam may show a large prostate or a hard, irregular surface. Because of PSA testing, prostate cancer is diagnosed during a rectal exam much less often.
The PSA blood test will also be used to monitor your cancer after treatment. Often, PSA levels will begin to rise before there are any symptoms. An abnormal digital rectal exam may be the only sign of prostate cancer (even if the PSA is normal).
The following tests may be done to determine whether the cancer has spread:
•CT scan
•Bone scan
The Gleason grade is how aggressive the prostate cancer might be. It grades tumors on a scale of 1 - 5, based on how different from normal tissue the cells are.
Often, more than one Gleason grade is present within the same tissue sample. The Gleason grade is therefore used to create a Gleason score by adding the two most predominant grades together (a scale of 2 - 10). The higher the Gleason score, the more likely the cancer is to have spread beyond the prostate gland:
•Scores 2 - 4: Low-grade cancer
•Scores 5 - 7: Intermediate- (or in the middle-) grade cancer. Most prostate cancers fall into this category.
•Scores 8 - 10: High-grade cancer (poorly-differentiated cells)
There are two reasons your doctor may perform a prostate biopsy:
•Your PSA blood test is high. See also: PSA
•A rectal exam may show a large prostate or a hard, irregular surface. Because of PSA testing, prostate cancer is diagnosed during a rectal exam much less often.
The PSA blood test will also be used to monitor your cancer after treatment. Often, PSA levels will begin to rise before there are any symptoms. An abnormal digital rectal exam may be the only sign of prostate cancer (even if the PSA is normal).
The following tests may be done to determine whether the cancer has spread:
•CT scan
•Bone scan
Prostate Cancer Symptoms
Sat, 13th August, 2011
The PSA blood test is often done to screen men for prostate cancer. Because of PSA testing, most prostate cancers are now found before they cause any symptoms.
The symptoms listed below can occur with prostate cancer (Most of the time these symptoms are caused by other prostate problems that are not cancer):
•Delayed or slowed start of urinary stream
•Dribbling or leakage of urine, most often after urinating
•Slow urinary stream
•Straining when urinating, or not being able to empty out all of the urine
•Blood in the urine or semen
•Bone pain or tenderness, most often in the lower back and pelvic bones (only when the cancer has spread)
Prostate Cancer Causes, incidence, and risk factors
Fri, 12th August, 2011
Prostate cancer is the third most common cause of death from cancer in men of all ages and is the most common cause of death from cancer in men over age 75. Prostate cancer is rarely found in men younger than 40.
People who are at higher risk include:
•African-American men, who are also likely to develop cancer at every age
•Men who are older than 60
•Men who have a father or brother with prostate cancer
Other people at risk include:
•Men exposed to agent orange exposure
•Men who abuse alcohol
•Farmers
•Men who eat a diet high in fat, especially animal fat
•Tire plant workers
•Painters
•Men who have been exposed to cadmium
The lowest number of cases occurs in Japanese men living in Japan (this benefit is lost after one generation of living in the U.S.) and those who do not eat meat (vegetarians).
A common problem in almost all men as they grow older is an enlarged prostate (benign prostatic hyperplasia, or BPH). This problem does not raise your risk of prostate cancer.
Minimally Invasive Prostate Cancer Therapy
Fri, 12th August, 2011
Is a High Intensity Focused Ultrasound, or HIFU, is a therapy that destroys tissue with rapid heat elevation, which essentially "cooks" the tissue. Ultrasound energy, or sound waves, is focused at a specific location and at that "focal point" the temperature raises to 90 degrees Celsius in a matter of seconds.
Male breast cancer
Fri, 12th August, 2011
is cancer that forms in the breast tissue of men. Though breast cancer is most commonly thought of as a woman's disease, male breast cancer does occur.
Male breast cancer is most common in older men, though male breast cancer can occur at any age.
Men diagnosed with male breast cancer at an early stage have a good chance for a cure. Still, many men delay seeing their doctors if they notice unusual signs or symptoms, such as a breast lump. For this reason, many male breast cancers are diagnosed when the disease is more advanced.
Male breast cancer is most common in older men, though male breast cancer can occur at any age.
Men diagnosed with male breast cancer at an early stage have a good chance for a cure. Still, many men delay seeing their doctors if they notice unusual signs or symptoms, such as a breast lump. For this reason, many male breast cancers are diagnosed when the disease is more advanced.
BLACK MEN AND PROSTATE CANCER
Fri, 12th August, 2011
All men should be concerned about prostate cancer, particularly as they age. Regular screening starting at age 50 is recommended for men who are at an average risk of developing prostate cancer. But if you have one or more risk factors and are at an increased risk of developing prostate cancer, early screening is especially important.
Men of African-American descent are at a significantly higher risk of developing prostate cancer than white men. Among black men, 19 percent — nearly one in five — will be diagnosed with prostate cancer, and five percent of those will die from this disease. In fact, prostate cancer is the fourth most common reason overall for death in African-American men.
Prostate Cancer in African-American Men: How Much Greater Is the Risk?
Researchers aren't exactly sure of the reasons why black men are at an increased risk of developing and dying from prostate cancer. "Unfortunately, right now we really don't know why African-American men are more likely to develop prostate cancer. We know that they are more likely to die from prostate cancer in part because of delayed diagnosis and in part because of limits in access to treatment," says Durado Brooks, MD, director of prostate and colorectal cancer at the American Cancer Society. A number of studies are under way in an attempt to better understand the causes.
And while African-American men are already at an increased risk for prostate cancer, their risk increases dramatically if there is a family history of prostate cancer. African-American men with an immediate family member who had prostate cancer have a one in three chance of developing the disease. Their risk rises to 83 percent with two immediate family members having the disease, and skyrockets to 97 percent if they have three immediate family members who developed prostate cancer.
Men of African-American descent are at a significantly higher risk of developing prostate cancer than white men. Among black men, 19 percent — nearly one in five — will be diagnosed with prostate cancer, and five percent of those will die from this disease. In fact, prostate cancer is the fourth most common reason overall for death in African-American men.
Prostate Cancer in African-American Men: How Much Greater Is the Risk?
Researchers aren't exactly sure of the reasons why black men are at an increased risk of developing and dying from prostate cancer. "Unfortunately, right now we really don't know why African-American men are more likely to develop prostate cancer. We know that they are more likely to die from prostate cancer in part because of delayed diagnosis and in part because of limits in access to treatment," says Durado Brooks, MD, director of prostate and colorectal cancer at the American Cancer Society. A number of studies are under way in an attempt to better understand the causes.
And while African-American men are already at an increased risk for prostate cancer, their risk increases dramatically if there is a family history of prostate cancer. African-American men with an immediate family member who had prostate cancer have a one in three chance of developing the disease. Their risk rises to 83 percent with two immediate family members having the disease, and skyrockets to 97 percent if they have three immediate family members who developed prostate cancer.
Colorectal (Colon) Cancer
Fri, 12th August, 2011
The third leading cause of cancer deaths in American men is colorectal cancer. This cancer is largely preventable through screening. Screening is recommended for men and women beginning at age 50. Screening tests for colorectal cancer can find precancerous polyps so they can be removed before they turn into cancer. Screening tests can also find colorectal cancer early, when treatment works best. People who have a family or personal history of polyps or colorectal cancer, inflammatory bowel disease, or certain genetic syndromes such as familial adenomatous polyposis (FAP) or hereditary non-polyposis colorectal cancer should talk to their doctors about screening earlier or more often than other people.
Prostate Cancer
Fri, 12th August, 2011
Prostate cancer is the most common cancer in men in the U.S., not counting skin cancer. It is the second most common cause of cancer death in men. While all men are at risk for prostate cancer, some factors increase risk. These include older age, a family history of prostate cancer, and being African American.
Not all medical experts agree that screening for prostate cancer saves lives. Currently, there is not enough evidence to decide if the potential benefits of prostate cancer screening outweigh the potential risks. Given the uncertainty about the benefit of screening, CDC supports informed decision making. Informed decision making occurs when a man—
•Understands the nature and risk of prostate cancer.
•Understands the risks of, benefits of, and alternatives to screening.
•Participates in making the decision to be screened at a level he desires.
•Makes a decision consistent with his preferences and values.
Not all medical experts agree that screening for prostate cancer saves lives. Currently, there is not enough evidence to decide if the potential benefits of prostate cancer screening outweigh the potential risks. Given the uncertainty about the benefit of screening, CDC supports informed decision making. Informed decision making occurs when a man—
•Understands the nature and risk of prostate cancer.
•Understands the risks of, benefits of, and alternatives to screening.
•Participates in making the decision to be screened at a level he desires.
•Makes a decision consistent with his preferences and values.
